How to Survive the New Wave of COVID-19
HIGHLIGHTS:
- Symptoms of COVID-19 include high fever, body aches and pain, sore throat, runny nose, coughing, and difficulty breathing. The new wave includes more severe symptoms, such as red eyes and hive-type rashes on the arms and legs.
- Persons considered high contact risk are those who have had contact with, and exposure to, patients with COVID-19. Such persons must quarantine for 14 days and be tested for infection 5 days after their contact with the patient. Low contact risk persons are those who have had contact with a high contact risk person. Low contact risk persons do not need to quarantine, but should wear a mask at all times and monitor themselves for symptoms for 14 days.
- Vaccination provides a level of protection against COVID-19 of 50-90%, which means that there remains some possibility of reinfection. However, vaccination reduces both the chance of reinfection and the severity of the disease.
As the COVID-19 situation in the country grows more and more severe, the total cumulative number of infections rises steadily each day. We are also seeing an alarming increase in deaths, with COVID-19 increasingly less discriminating of age or gender and more easily spreading to all. In addition to our “new normal“ lifestyles, it cannot be denied that vaccination is a major hope for the Thai people in this current crisis.
How much longer will we have to live with COVID-19?
Looking at the growing number of infections worldwide, COVID-19 is likely to stay with us for another year. That said, if we can achieve vaccination of more than 70% of the world’s total population we should achieve “herd immunity,” or at least provide enough immunity to fight COVID-19 to a greater extent. Based on a vaccination rate of 15 million doses a day, the global population of more than 7 billion people would require about 1,000 days (3 years) to fully vaccinate. In order to achieve herd immunity more quickly, therefore, it is imperative that we speed up the vaccination process; that is, a higher number of doses need to be given per day so as to shorten the overall vaccination time.
Where Am I in this Pandemic?
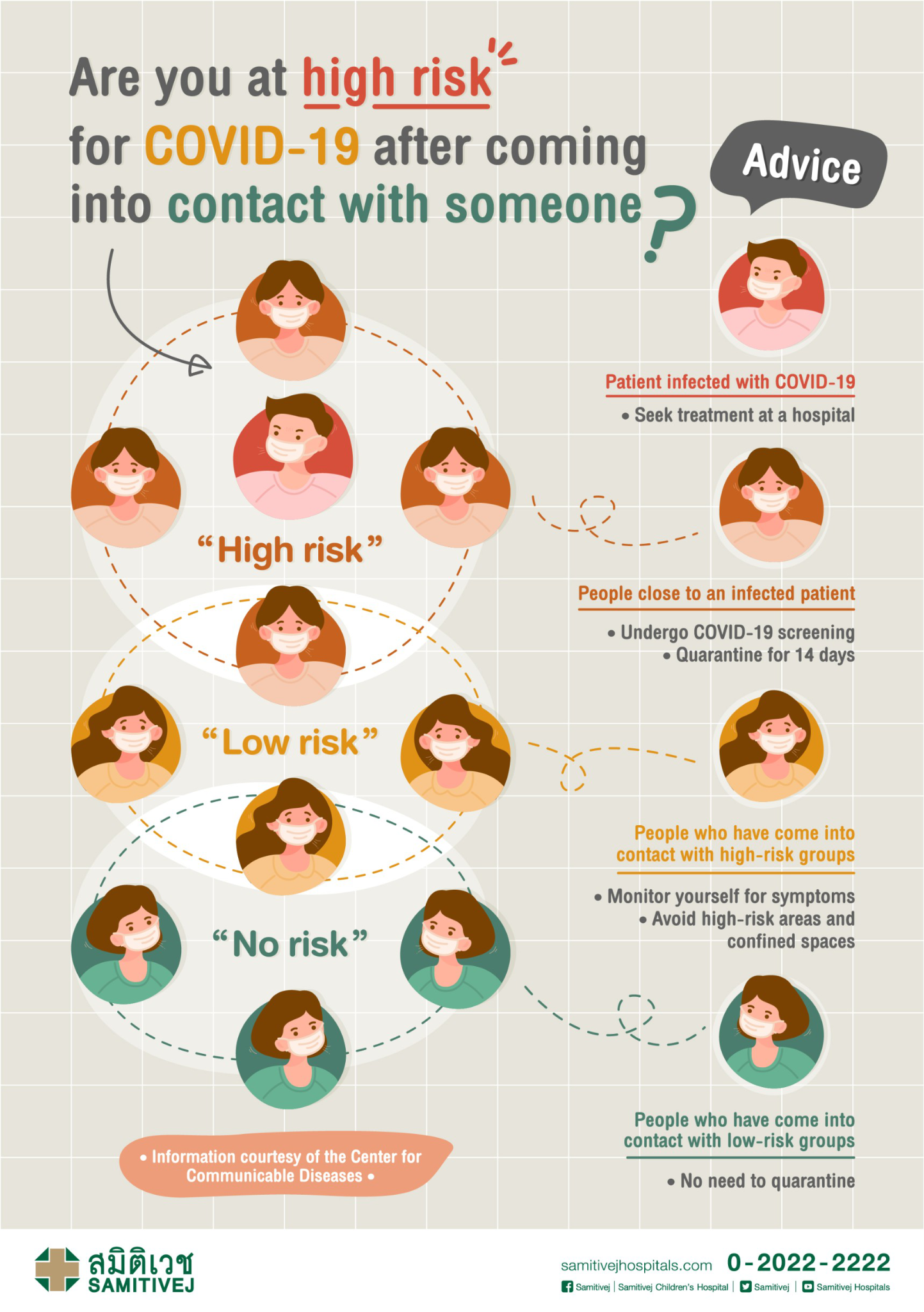
When you hear that someone close to you has been infected with COVID-19, you may wonder how much you are placed at risk as a result.
Group 1: If Person A is a COVID-19 patient and another person comes near to, or in close contact with, Person A, that second person would be called a high-risk contact (Person B). This means having been in close proximity (within 1 meter) to the patient for a sustained period of 15 minutes or more, with or without masks. Person B is advised to quarantine for 14 days with no contact or close proximity to anyone else, wear a mask, wash their hands frequently, and be tested for infection on the 5th day after their first contact with Person A. Testing prior to the 5th day after first contact with the patient is not recommended, as the test could produce false negative results if the virus is still in its incubation period. Additionally, in the case of a false negative, Person B could mistakenly believe that they are COVID-free and unknowingly infect others as a result.
Group 2: A person who has been in close contact with someone in group 1 (Person B) would be considered a low-risk contact (Person C). For example they may have walked past one another, spoken to each other for less than one minute while wearing a mask and without any physical contact, remained 1-2 meters apart, or may have been a work colleague of someone in group 1, etc. Those in this low-risk contact group (Person C) are advised to wear a mask and to avoid crowded or at-risk locations, as well as to observe their symptoms for up to 14 days. However, they do not need to quarantine.
Group 3: Those considered not-at-risk may be someone in the same community or living in the same condo building as a COVID-19 patient but who has had no contact with them. As a basic precaution, it is recommended that they wear a mask, wash their hands frequently, and keep a safe distance from others. However, quarantine is not necessary.
How to self-isolate at home for safety
Hospital bed shortages are considered a major problem at the moment (April 26, 2021) due to the large number of positive cases being detected all at once. However, while the number of beds available in each hospital may be limited, there are other options for treating those with positive test results. If someone tests positive for COVID-19 but is unable to find quarantine facilities due to hospital bed shortages or hospital overcrowding, it is possible to self-quarantine at home with self-care such as taking fever reducers, nasal decongestants, and cough syrup (depending on the symptoms). Most importantly, these individuals should drink a lot of water—at least 3 liters per day—while honey and lemon can also be added. Taking vitamin C to boost the immune system and eating lots of fruits and vegetables and other healthy foods is a good idea, while good self-observation should be practiced throughout.
In addition, for anyone self-quarantining at home, ensure you have a clear separation of areas in the house if you are living with other people. Stay at least 2 meters away from others at all times, and don’t share dishes, utensils, or glasses, etc. If you have to share a bathroom with others in the house, the main thing to keep in mind is cleanliness of any points of contact, especially contact points where lots of germs or bacteria can be found, such as doorknobs, basins, faucets, shower hoses, etc. After using any of these, take an alcohol pad, alcohol wipe, tissue moistened with alcohol, or a cloth dampened with an antiseptic/disinfectant, and wipe clean everything that you touched. Make sure to use the bathroom at different times than others in the house. Additionally, after you have used the toilet, make sure to first close the toilet lid before you flush, as there are reports that the virus can be mixed with urine and the infection can spread if the toilet is flushed without first closing the lid.
What are the symptoms of this new wave of the virus and when should I see a doctor?
The first major symptom of this wave of COVID-19 is a high fever starting from the very first day. Alternatively, if not on the first day, then the fever will appear on day 4 or 5, along with achiness in various parts of the body. Some people then begin to experience more severe symptoms, such as intense body, joint, and muscle pain, increased coughing, sore throat, trouble breathing, or a feeling of tightness in the chest. Any of these symptoms should be taken as signs that the condition is getting worse and you need to be under the supervision of a doctor.
On the other hand, if you are tested and the results are positive but you have no symptoms or very few or minor symptoms, such as a common cold and no fever, there are alternative options for quarantine such as accommodations that have been characterized as “hospitels.” The basic principle of a “hospitel” is that there are hospital staff stationed at the hospitel/hotel to check temperatures and assess symptoms each day. If any abnormalities are found, you would immediately be sent to a hospital.
What are the differences between a common cold and COVID-19?
The symptoms of a common cold are clear mucus and runny nose, sometimes low fever of about 37 degrees Celsius (no higher than 37.8), slight cough, and sore throat. Symptoms generally disappear after about 3-5 days, and there is usually no accompanying body pain.
Symptoms of COVID-19 are a high fever of 37.8 degrees Celsius and above, more body pain and achiness like with the flu, and, for some, bone and joint pain, sore throat, runny nose, coughing, etc. The new wave has also brought with it an increase in symptoms such as red eyes, blotchy or hive-type rashes on the arms, legs, and body (found in approximately 10% of cases); and, for some patients, clear blisters similar to chicken pox.
Treatment Methods for COVID-19 Patients
To date (as of April 26, 2021), there are no approved antiviral drugs specific to COVID-19. Available treatment, instead, focuses on management of symptoms. For example, fever will be treated with fever reducing drugs, coughing with cough suppressants, congestion or runny nose with decongestants, etc.
However, if symptoms worsen, for example if lung X-rays begin to show abnormalities, if there is a high fever, and if the patient also has other chronic or underlying diseases such as lung disease, kidney disease, liver disease, heart disease, obesity, diabetes, or if the patient is pregnant, these would qualify a person as being high-risk. In such cases, they should immediately contact a hospital for treatment and the doctor will provide treatment using both injectable and oral medications.
Side Effects or Allergic Reactions After Vaccination
Because both the disease itself and the vaccines being used against COVID-19 are fairly new, there is not a large amount of data available to be studied. As a result, it’s natural that many people might feel concerned about being vaccinated. Doctors recommend, however, that if you have the opportunity to be vaccinated you should take it, regardless of the brand, as some vaccination and protection is better than none at all. If you are vaccinated, you can be confident you will be protected with at least 50% efficacy. Additionally, approved vaccinations are safe with very few side effects. After receiving the injection, you may feel some soreness around the injection site, a little weakness and fatigue, or have a low fever, which will last for just about 1-2 days. Also, as mentioned above, 70% of the world’s total population would need to be vaccinated in order to achieve global herd immunity and protection against the disease. As such, anything we can do to accelerate vaccinations is also helping us personally to be better protected against COVID-19.
At present (June 2021), there is no evidence of death as a result of the vaccine. However anaphylaxis has occurred in approximately 2 to 5 people per million vaccinated.
Vaccination and Reinfection
After being vaccinated, you will be protected against COVID-19 by 50-90%, which means there is still some possibility of reinfection. However, vaccination reduces both the chance of reinfection and the severity of the disease. Therefore, if reinfection were to occur, the symptoms would likely be mild or nonexistent.
As there is still some chance of reinfection after vaccination, and because under current circumstances the COVID-19 pandemic is considered to be “uncontrolled,” it is recommended that you continue to wear a mask, wash your hands regularly, practice social distancing, and avoid activities that require you to be in large groups, such as crowded places or areas, or pubs and bars, etc., that are enclosed spaces with a lot of shouting and chatting, all of which increase the risk of infection.
Is there a recommended interval between getting the COVID-19 vaccine and the flu vaccine?
The vaccines should be spaced about 2 weeks apart. The COVID-19 vaccine and any other vaccine should not be given at the same time because if any side effects do occur it will be impossible to identify which vaccine was the cause.
Finally, we should all practice good self-observation in regard to whether or not we have any history of exposure to at-risk groups, and we should always be on the lookout for possible symptoms. If you do experience any abnormal symptoms, such as a rash, etc, don’t panic—a rash or any other symptom doesn’t necessarily mean that you have COVID-19. COVID-19 usually exhibits several symptoms at the same time, for example a rash along with a high fever and body pain. Symptoms should be monitored along with observations of your history of exposure to any at-risk groups.
For both economic and other reasons, it will be difficult for the country to be put on lockdown every time there is a surge in COVID-19 cases. As such, anything we can do to get back to a “new normal” by wearing a mask, washing our hands frequently, and, most importantly, getting vaccinated to strengthen our defenses against COVID-19, will not only help build up our bodies’ immune systems but also ultimately end the outbreak of the disease.
Related
articles