A Potential Solution for Cervical Cancer: 2-, 4- and 9-strain HPV vaccines
HIGHLIGHTS:
- Twenty-four women a day are diagnosed with cervical cancer in Thailand, with most of that number coming from the 35–44 year-old age group.
- Almost 100% of cervical cancer cases can be traced back to an HPV infection, which means that cervical cancer can be prevented with an appropriate vaccination program alongside regular screening.
- Even just one sexual partner increases a woman’s risk of contracting HPV due to this virus being so easily spread. Indeed, 80% of the population have asymptomatic HPV infections, so it is easy to see how just one sexual partner can pass it on.
What is HPV?
HPV stands for human papilloma virus, which can cause infections to occur throughout the body. This virus has over 100 strains, with the strains considered as high risk due to their potential to develop into cancer as follows: 16, 18, 31, 33, 35, 45, 52, and 58. Low risk strains, on the other hand, are those that may cause genital warts, including strains 6 and 11.
HPV is a common factor behind the onset of several forms of cancer, such as cervical cancer, vaginal cancer, vulvar cancer, penile cancer, anal cancer, and oral cancer.
Once contracted, the human papilloma virus is able to conceal itself for decades without causing any symptoms whatsoever. It is therefore capable of spreading to other organs without the patient’s knowledge, with symptoms generally only presented once an infection has already taken hold. Moreover, it has been found that the human body is less able to fight off the virus as it ages, which can lead to a permanent HPV infection that increases the patient’s risk of developing cancer in later life.
Preventing an HPV infection
HPV infections can be prevented with a vaccination program, with the following 3 types currently available throughout Thailand:
| HPV vaccine | HPV Strains protected against | |
| High-risk type | Low-risk type | |
|
16,18 |
- |
|
16, 18 |
6, 11 (genital warts) |
|
16, 18, 31, 33, 45, 52, 58 (An additional 5 strains) |
6, 11 (genital warts) |
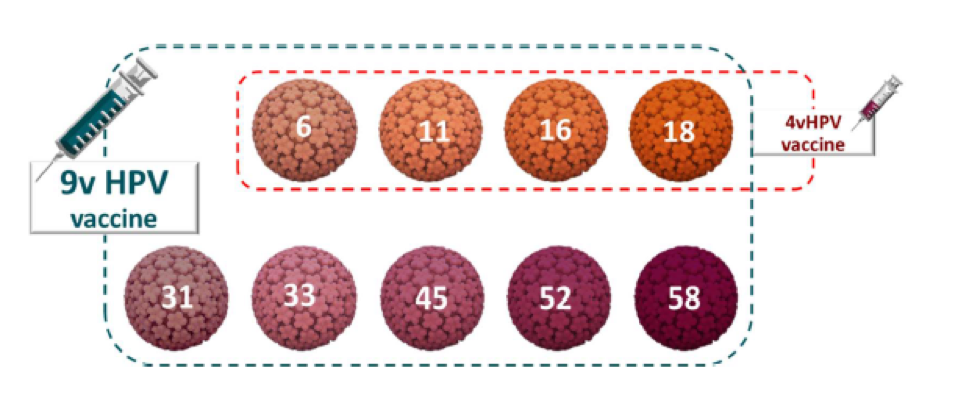
Why is it necessary to vaccinate against 9 strains of HPV?
A 9-strain HPV vaccine offers more comprehensive protection for patients who may already have contracted certain strains of HPV, while also preventing infection from additional strains.
The 9-strain HPV vaccine can be administered to both males and females between the ages of 9 and 45 years, while this vaccine can also help to protect against the following conditions:
| Protects against | HPV strains causing the disease |
| Cervical cancer, vaginal cancer, vulvar cancer, anal cancer, and oral cancer |
16, 18, 31, 33, 45, 52 and 58 |
| Precancerous lesions related to cervical cancer, vaginal cancer, vulvar cancer, and anal cancer |
6, 11, 16, 18, 31, 33, 45, 52 and 58 |
| Genital warts |
6 and 11 |
Studies into the causes of diseases, including cancers, resulting from various HPV infections have found that the 9-strain HPV vaccine offers up to 90% cervical cancer coverage. It also provides protection against precancerous lesions associated with cervical cancer, vaginal cancer, and vulvar cancer, of which up to 97% of cases are caused by the following strains of HPV in patients with no prior history of an HPV infection: 31, 33, 45, 52, and 58.
HPV 9 vaccine advice
- Male and female recipients aged 9–14 years
Two injections, with the second following 6–12 months after the first. This is the age group for which the vaccine can be of most benefit, while the 2-injection course suited to under 15s can also reduce the costs involved with vaccinations. - Males aged 16–26 years and females aged 16–45 years
Three injections, with the second following 1-2 months after the first, and the third following 4 months after the second. It is recommended that the second injection be administered at least 1 month after the first, while the third should be at least three months after the second and at least 5 months after the initial injection. Crucially, all 3 injections must be carried out within a 12-month period.
Related
articles