

| ATK: Negative results (No infection found at the time of examination) |
-If it is a high-risk contact or there is any risk history, the test should be repeated5-7 days after the first test. The patient should be quarantined for 14 days for observation. -If there are signs of respiratory symptoms, the patient should make an appointment for doctor consultation and treatment. |
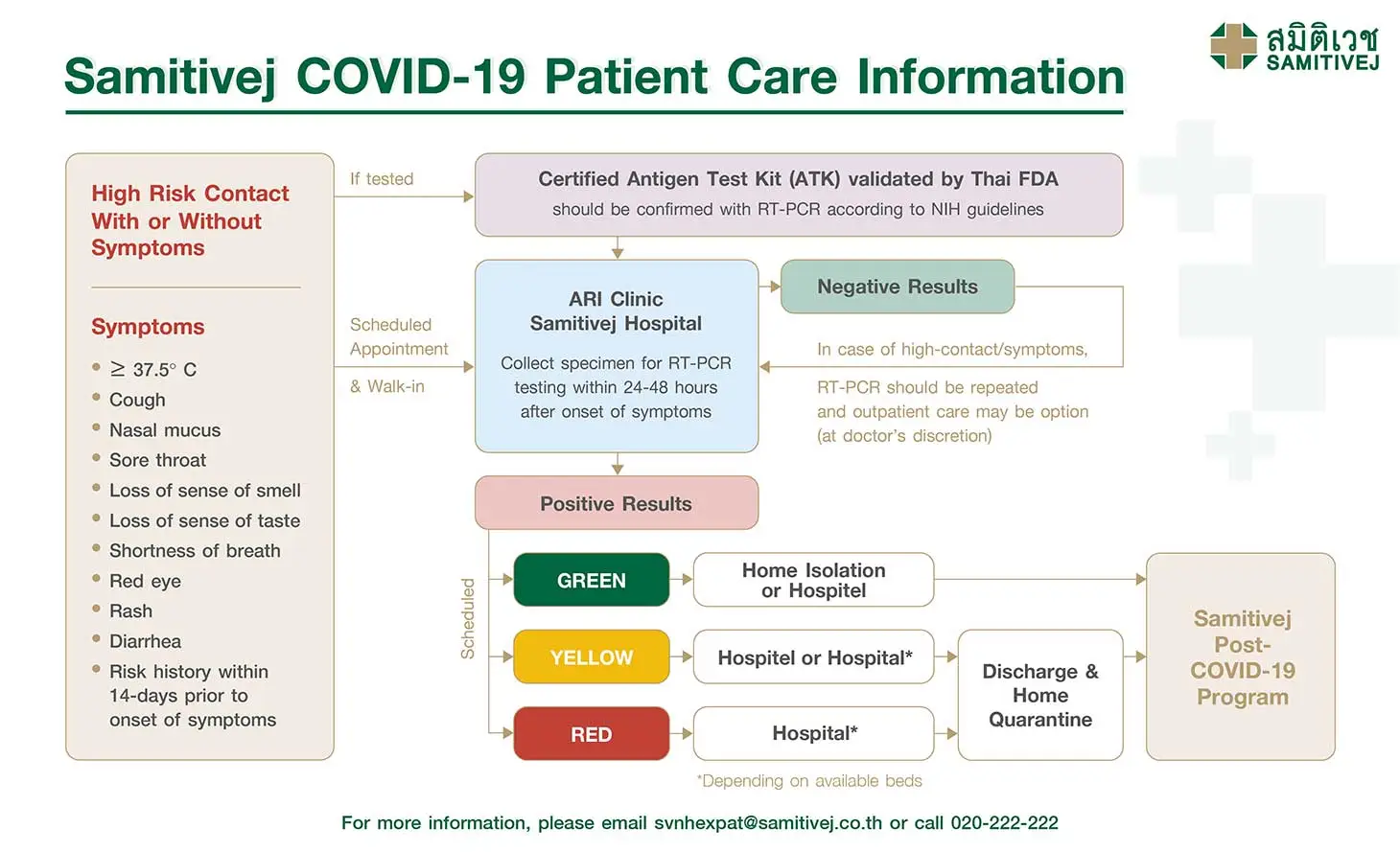
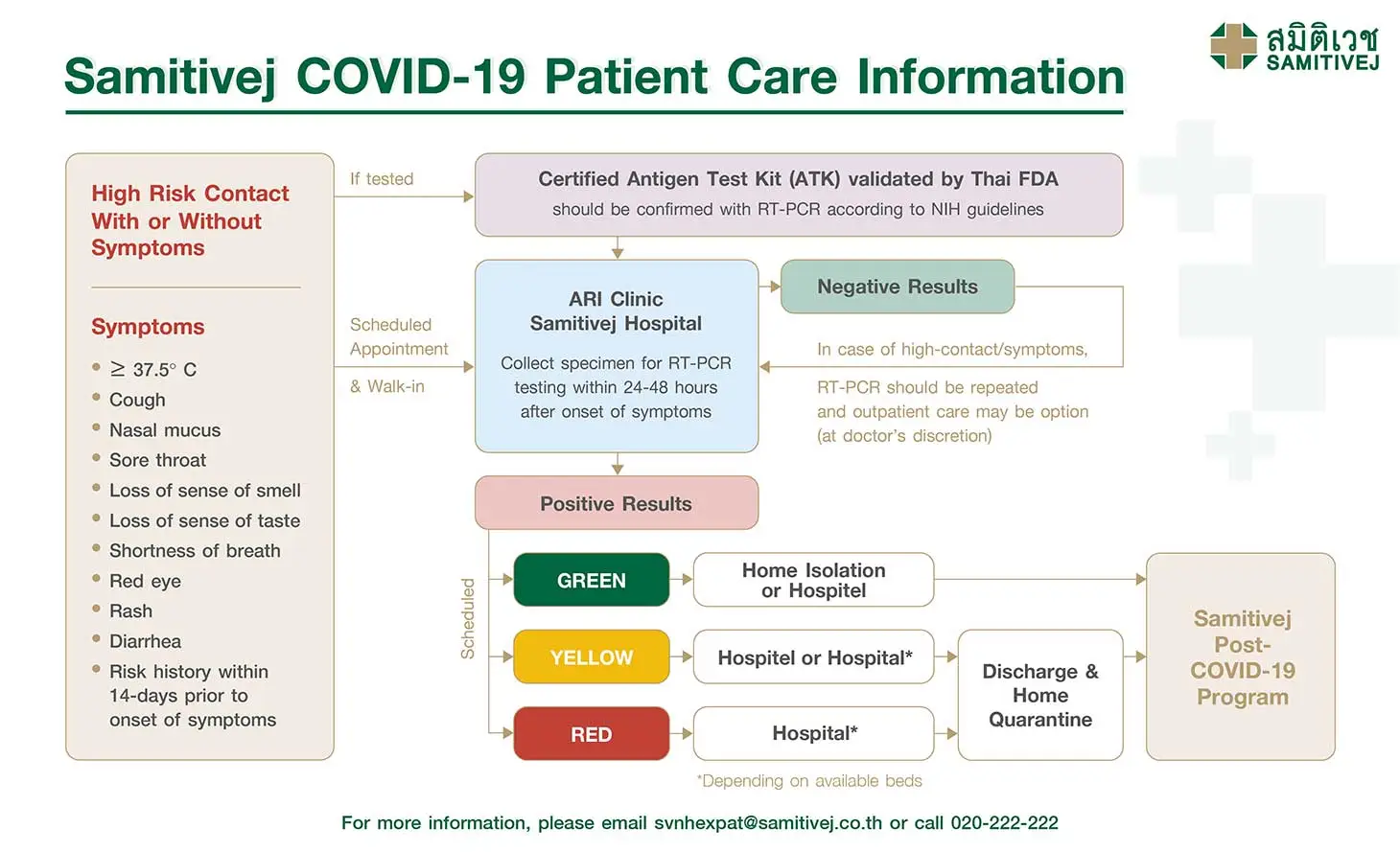
| ATK: Positive results | The patient should make an appointment for doctor consultation and treatment. Guidelines require that a doctor needs to confirm the results with RT-PCR testing. |
To schedule appointment, please contact svnhcontact@samitivej.co.th
Steps for RT-PCR testing for SARS-CoV-2:
RT-PCR Cost:
Samitivej Sukhumvit Hospital: THB 4,000 including doctor’s fees and outpatient service fees but excluding medicines or other procedures as ordered by the doctor.
The doctor will consider appropriate treatment if patients have any symptoms. Outpatient care can be a treatment option if a bed is not available. Patients with high-risk contacts need to repeat RT-PCR testing as indicated by the doctor.
| Patient with symptoms: high-risk contact | Doctors will decide case by case when patients need to repeat the RT-PCR testing. Home-quarantine for 14-days after contact with a confirmed case. |
| Patient with symptoms: low-risk contact | Home isolation may not be required, but patient must follow disease control measures i.e. masking, hand hygiene, distancing and separating personal items |
| Asymptomatic patient: high-risk contact |
Patients must test for SARS-CoV-2 again either 7 days after the first test or 13 days after the last contact with the confirmed case, whichever comes first. |
The doctor will contact the patient directly with test results within 24-48 hours. Patients will be classified by the doctor who performed the RT-PCR testing according to their clinical symptoms. In each category, doctors will consider each case separately to decide whether the patient should receive treatment at home (Home Isolation Program), in a hospitel or in the hospital.
Some patients will have to make an appointment for further diagnostic tests including chest X-ray and/or blood testing. Doctors will develop a treatment plan based on lab results. Qualified patients who can be monitored and treated in hospitel will be informed of their check-in date and the estimated number of days they will stay in the hospitel.
| Green | - No symptoms or mild symptoms such as fever, dry cough, runny nose, conjunctivitis, or skin rashes - Age under 60, no underlying diseases |
Home Isolation or Hospitel |
| Yellow | Mild symptoms but experiencing breathing difficulty or rapid breathing, and one or more underlying risk factors:
|
Hospitel or Hospital* |
| Red | Breathing difficulty or shortness of breath. Chest X-ray reveals severe pulmonary infiltration. COVID-pneumonia (oxygen saturation <96% or oxygen saturation decrease > 3% after exertion (exercise-induced hypoxemia)) | Hospital* |
*Depending on available beds
Patients who had RT-PCR testing at Samitivej Sukhumvit and are in the green category will be offered a Home Isolation Program, which will be closely monitored by the hospital as follows:
14-day Home Isolation Package Cost:
Due to the limited number of beds, Samitivej Sukhumvit Hospital collaborates with Adelphi Suites and Serviced Apartment Bangkok (Sukhumvit 8) and Hope Land Hotel (Sukhumvit 8). Registered nurses are on standby at the hotels around the clock. Patients can have a video call consultation with a doctor thru Samitivej Virtual Hospital. Patients can only choose the hospitel option when there are rooms available in these two hotels.
14-day Hospitel Cost:
When a patient’s condition improves, they are allowed to move to home quarantine but must maintain the principles of preventing infection according to the new standards.
There is no need to repeat testing with RT-PCR, antigen or antibody detection in patients who are already confirmed cases, including when they are discharged, except for the purpose of research (the researcher must clearly explain this to the patient).
After discharge and after completing the quarantine period, patients should follow new normal practices including wearing masks, hand washing, social distancing, and avoiding crowded or poorly ventilated areas.
(from date of onset of symptoms, or date of positive test result if asymptomatic)
In some cases, during the initial stages of a COVID-19 infection recovery, patients may experience severe inflammation throughout the body causing a membrane or white spots, visible on an X-ray, to form on the lungs. However, not many white spots are found.
Other symptoms seen in some patients recovering from a COVID-19 infection are feelings of fatigue, weakness and exhaustion. In addition, some patients who have recovered from a COVID-19 infection have experienced a 20–30% reduction in pulmonary function, but this can be reversed with treatment.
Samitivej offers pulmonary function rehabilitation and health recovery programs for patients with no severe respiratory conditions who are recovering from COVID-19.
Learn more about pulmonary rehabilitation following recovery from a COVID-19 Infection here.
For more information, please contact svnhcontact@samitivej.co.th.
Once a patient recovers from a COVID-19 infection, their lungs, which are directly impacted by the infection, are likely to be partially damaged. However, did you know that other bodily systems, such as the heart and coronary artery system, are also affected and that the patient’s overall physical capabilities may also suffer?
The lungs may exhibit scarring or tissue damage, which could lead to the patient being unable to take a full, deep breath, thus leaving them feeling breathless and tiring easily. The heart, on the other hand, may be more prone to disease, whether as a result of an increased workload on the immune system having a negative effect on the heart muscle or the virus itself infiltrating and directly impacting the heart muscle. This means that recovering COVID-19 patients are at greater risk of developing certain heart conditions in the future, including heart failure, arrhythmia, and other heart conditions. Moreover, the overall health of some recovering patients has also been found to be significantly affected by the infection, with patients reporting exhaustion, fatigue, not feeling fresh and a general feeling of weakness. These issues are a result of severe inflammation throughout the body as a result of the immune system being unable to return to its former, healthy state. Additionally, the stress and anxiety felt by patients experiencing a COVID-19 infection, as well as side effects from medication or even repeated bacterial infections caused by prolonged use of immunosuppressive drugs, are all factors that can disrupt the recovery process. This means that patients may not feel 100% recovered for quite some time after they leave the hospital.
Regular health screening, including pulmonary function tests, heart function analysis and inflammation screening, a comprehensive rehabilitation program that includes breathing exercises, light exercise, regular testing of vitamin levels and antioxidant levels, vaccines, and vitamin supplements to boost immunity levels, and other techniques to improve health are essential to patients recovering from a COVID-19 infection. Taking such steps can help patients assess their health and plan for further rehabilitation so the body and its organs can be restored and work better, enabling patients to make a rapid return to their daily lives and improve their overall quality of life.
Learn more about Post-COVID-19 Health Rehabilitation here.
For more information, please contact svnhcontact@samitivej.co.th.
After an infection with SARS-CoV-2, most people—even those with mild infections—appear to retain some protection against the virus for at least a year, according to a recent follow-up study of recovered patients1. This, along with other research, demonstrates that vaccinating individuals after they have recovered from COVID-19 substantially enhances their immune response and confers strong resistance against variants of concern, including the Delta variant.
If you wish to analyze your level of immunity before receiving a COVID-19 vaccine, learn more about COVID-19 antibody testing here.
articles