Pediatric Neurosurgery Center
Neurosurgical disorders from newborn infants to 18-year-olds. Our expert team of pediatric neurologists, genetic physicians, pediatric neurosurgeons and other pediatric specialists are also available for consultation on any abnormalities and our teams of anesthetists are on hand for effective pain relief during treatment.
Our team of nurses in the Out-Patients Department, the Newborn Intensive Care Unit (NICU), and the Pediatric Intensive Care Unit (PICU) are all experienced and highly trained to provide the best of care. Patients are carefully evaluated to find the underlying causes of any symptoms before our specialists decide on the best treatment with the optimal outcome.
- Diagnostic technologies and all necessary investigations such as EEG, EMG, CT Scans, MRI, MRA, MRV and Cerebral angiograms for pediatrics that enable us to arrive at a complete treatment plan and the best treatment option for each patient.
- Treatment and care of children suffering from neurological disorders such as chronic headaches, encephalitis, epilepsy, meningitis, intracranial hemorrhages, brain abscesses, subdural empyema, hydrocephalus, arachnoid cysts, brain tumors, congenital brain and spinal cord anomalies, craniosynostosis, etc.
- Brain and spinal surgery for children from newborn infants to 18-year-olds by our pediatric neurosurgeons (Laminectomy, Craniotomy and Craniectomy)
- Shunt surgeries (VP shunt, VA shunt, Cysto-Pleural shunt, Syringo-Pleural shunt)
REAL CLEAN MEANS
Post-treatment advice
Hydrocephalus
Hydrocephalus is a very serious condition caused when an excess supply of cerebrospinal fluid (CSF) builds up in the ventricles of the brain.
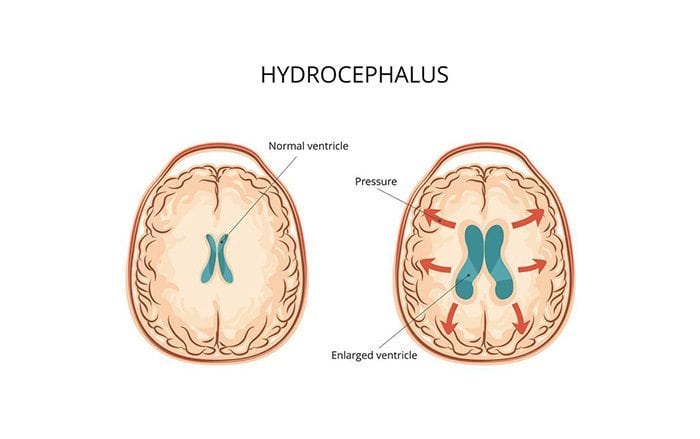
The brain and spinal cord are surrounded by CSF and when the normal circulation of CSF is prevented in some way, it collects in the ventricles and they increase in size, building pressure inside the head, which causes hydrocephalus. There are two varieties of hydrocephalus: communicating hydrocephalus and non-communicating hydrocephalus. Communicating hydrocephalus is so-called because the CSF can still flow among the open ventricles, but is blocked when it exits them. Non-communicating hydrocephalus is also known as “obstructive hydrocephalus” because, in these cases, the flow of CSF is blocked in one or more of the narrow passages between the ventricles. Frequently, the reason for this is “aqueductal stenosis”, when the aqueduct of silvius, the passage between the third and fourth ventricles in the center of the brain, narrows. Some hydrocephalus is congenital, that is, it is present at birth. It may have been caused by something that happened when the fetus was developing in the womb or by genetic abnormalities. Hydrocephalus which develops at any time after birth is called acquired and may affect people at any age. Injury or disease may be the cause of acquired hydrocephalus. It is possible for a child to develop hydrocephalus which does not reveal its symptoms until adulthood, although this is rare. Often, though not in every case, this type of hydrocephalus is caused by aqueductal stenosis.
How does a doctor diagnose hydrocephalus?
Once a medical practitioner suspects some type of hydrocephalus to be present, he or she will carry out various tests to ensure the diagnosis is correct and to ascertain the suitability of the patient for shunt treatment.
How is hydrocephalus treated?
A shunt, which is a surgically implanted device that drains CSF from the brain into another part of the body where it can be absorbed, is the only treatment available for hydrocephalus.
Hydrocephalus: Recommendation for Parents
Knowing the symptoms
There are a number of different symptoms for hydrocephalus that may present themselves during an individual’s lifespan, starting from unborn children all the way to the elderly. Throughout a woman’s pregnancy, a scheduled ultrasound will normally be able to identify either enlarged ventricles or spaces within the child’s brain. For infants, the most noticeable symptom is an abnormal enlargement of their head. As the child grows, the symptoms will become less physically apparent, but rather present themself in the form of nausea, vomiting, headaches or blurry vision.
Dizziness and vision problems remain the primary symptoms of hydrocephalus from teenage years right through until middle age. For the elderly, if they are diagnosed with normal pressure hydrocephalus (NPH), the symptoms are generally more severe. This often includes the deterioration of bodily functions such as walking, trouble developing coherent and cogent thoughts, and poor bladder regulation.
To ensure early diagnosis and treatment, it is important to recognize the warning signs when they present themselves. They include:
Infants and Children
- Abnormal enlargement of the head
- A noticeable tenseness and bulging of the fontanel (soft spot)
- Conspicuous veins on the scalp
- A feeling of ‘separation’ between the skull bones
- Headaches, nausea and blurry vision
- Drowsiness, vomiting and irritability
- A tendency to deviate their eyes downwards
Teenagers
- Prolonged and consistent headaches
- Inability to think clearly or to concentrate
- Trouble walking
- Decreased ability to control bladder or incontinence
Post-treatment advice
It is vitally important that you attend all well-baby visits with your child. Your child’s development will be monitored by your child’s doctor during these regular visits, at which time, he or she will check the following:
- Overall body growth, head size and rate of head growth
- Muscle strength and tone
- Posture
- Motor skills appropriate to age
- Coordination
- Sensory functions – hearing, sight and touch
Team of Specialist
Panu Nacharoong, M.D. – Pediatric Neurosurgeon
- M.D., Faculty of Medicine of Prince Songkla University, 1998
- Diploma of Thai Board of Neurosurgery, Bhumibol Adulyadej Hospital, Royal Thai Air Force (RTAF) , 2003
- Certificate of Pediatric Neurosurgery , Taipei Veterans General Hospital, Taiwan 2009
- Certificate of The Asian Australasian Advanced course in Paediatric Neurosurgery (AAACPN) Singapore, Taiwan, India ; 2007,2008,2009
- Specializes in: Pediatric brain tumor surgery, Pediatric Neurosurgery
Nunthasiri Wittayanakorn, M.D. – Pediatric Neurosurgeon
- M.D., Faculty of Medicine, Khonkaen University
- Diploma of Thai Board of Neurosurgery, Bhumibol Adulyadej Hospital, 2012
- Diploma of Neurological Surgery, The royal children hospital, Melbourne , 2016
Somjit Sri-Udomkajorn, M.D. – Pediatric Neurologist
- M.D., Faculty of Medicine, Chulalongkorn University, 1989
- Diploma of Thai Board of Pediatrics, Queen Sirikit National Institute of Child Health, 1995
- Specializes in: pediatrics; pediatric neurology
Navarat Rungteeranon, M.D. – Pediatric Neurologist
- M.D., (First class honours), Faculty of Medicine, Chulalongkorn University, 2000
- Diploma of Thai Board of Pediatrics, Faculty of Medicine Chulalongkorn University, 2008
- Specializes in: pediatrics, pediatric neurology
Apasri Lusawat, M.D. – Pediatric Neurologist
- M.D., (Honors) Faculty of Medicine, Ramathibodi Hospital, Mahidol University
- Diploma of Thai Board of Pediatrics
- Certificate in Pediatric Neurology, The Royal College of Pediatricians of Thailand
